Guys have signs of papillomas. Human papillomavirus (HPV): how does the disease manifest itself in men? Surgical treatment

The human papillomavirus (HPV) is widespread throughout the world. It equally often affects both men and women. More than 200 types of papillomaviruses are known. The danger is that they can cause the development of cancer.
- 1 Anogenital warts: lesions in the form of spots, papules and more rare forms: Bowen's disease, bowenoid papulosis, Buschke-Levenstein's giant condyloma.
- 2 Extragenital papillomas and warts:
- Damage to the skin of other localization: flat, vulgar, plantar warts, epidermodysplasia verruciform, non-warty skin formations, etc.
- Papillomas of mucous membranes: larynx, conjunctiva of the eye, oral mucosa, etc.
- 3 Dysplasia, precancerous conditions.
- 4 Cancer of the anus and anal canal, cancer of the penis, etc.
- 1 Latent form (has no external signs, proceeds hidden, is detected in a laboratory study).
- 2 Subclinical form (erased manifestation of the disease).
- 3 Clinical form (classic symptoms of infection in the form of neoplasms, dysplasia).
- 1 Early onset of sexual activity, a large number of partners and their frequent change.
- 2 Neglect of barrier contraception (condoms).
- 3 Concomitant sexual infections (chlamydia, gonorrhea, genital herpes, syphilis, trichomoniasis).
- Pain, cramps, discomfort during urination.
- Unpleasant sensations during intercourse, sometimes extremely painful.
- Bleeding of genital warts with the appearance of long-term non-healing cracks.
- Difficulty emptying the bladder and ejaculation with the appearance of large warts in the urethra.
- 1 Injury with the addition of a secondary infection.
- 2 Bleeding.
- 3 Phimosis or paraphimosis (narrowing foreskin).
- 1 In the perineum, near the anus, on the foreskin, body of the penis, scrotum. They look like papules (dense nodules) without protrusions and growths.
- 2 They can affect not only the skin and mucous membranes of the genital organs, but also be located on other parts of the body: soles and palms, limbs, neck, face and head, torso. Palmar-plantar warts affect the skin of the feet and palms, have dark blotches on their surface, which distinguishes them from ordinary corns, and cause inconvenience when walking.
- 3 Filamentous are well known to many people and are located on the skin of the neck, eyelids, face, chest, and forearms. They are thin, mobile, flesh-colored protrusions; among patients, the name “hanging mole” is found.
- 4 Vulgar and flat warts are small (up to 0.5 cm), often multiple and have growths. Usually found on the back of the hand and foot (not to be confused with the palmar-plantar!).
- 5 Cystic, mosaic also often localized on the plantar surface of the foot, differ in structure and appearance.
- 1 Ulceration of the surface.
- 2 Bleeding.
- 3 Roughness, tuberosity, uneven staining, sores.
- 4 Formation of fistulas with purulent discharge.
- 5 General symptoms (subfebrile temperature, weakness, enlargement of regional lymph nodes).
- 1 The human papillomavirus cannot be completely removed from the body. In some of the infected, the virus is eliminated without the participation of the doctor and the patient.
- 2 External cosmetic defects (warts, warts and papillomas) are removed using one of the following methods.
- 3 In addition, interferon preparations can be prescribed to strengthen immunity and fight infection, as well as to reduce the number of relapses and complications.
- 4 HPV-infected high oncogenic risk shows dynamic monitoring. It is important to notify the woman of the possibility of transmission of the virus and to monitor her. HPV types 16 and 18 are responsible for most cases of squamous cell carcinoma of the anus and cervix.
Show all
1. How can you get infected?
The infection is usually transmitted sexually. There is also data on contact-household infection through a handshake, swimming pool, linen, hygiene items. Transmission of infection during childbirth from mother to child is possible (vertical route).
HPV infects epithelial cells, penetrates into the deepest layers of the skin or mucous membranes, it can persist in them for a long time. In many, the virus is eliminated from the body on its own within 12-24 months after infection.
Interesting! About half of the adult sexually active population of the planet is infected with some type of papillomavirus!
The peak incidence occurs at 17-29 years of age, at an older age the risk of infection persists.
2. Classification
According to the flow, they distinguish:
It should be clarified that in the practice of a doctor the latent form is more common. separate group form persons with severe immunodeficiency (HIV-infected, conditions after organ transplantation, etc.), debilitated patients, it is in them that it is much more difficult to treat the infection.
3. Risk factors
These are conditions that increase the chance of contracting papillomavirus. The following risk factors can be distinguished:
Avitaminosis, other somatic diseases and factors leading to immunodeficiency increase the likelihood of clinical manifestations.
4. Symptoms of HPV in men
The incubation period of HPV infection is about 3-6 months, sometimes it can be extended up to a year. It is believed that in 90% of all cases, self-healing and complete ridding of the body of the human papillomavirus occurs. In another part of the infected men, clinical signs of infection of varying severity appear, which depends on the type of virus, its titer, and the state of immunity.
The most common manifestations in men are warts and papillomas.
4.1. Genital warts
They are elongated, light pink growths on the skin and mucous membranes, which have a characteristic structure and pattern. It is sometimes said that outwardly warts look like cauliflower.
Most often they appear in places subject to the greatest friction during intercourse: the glans penis, urethra, foreskin (bridle, inner surface of the leaf), anus (during anal intercourse). Condylomas are characteristic for 1-6, 10, 11, 16, 18, 30, 31, 33, 35, 39-45, 51-59, 70, 83 types of human papillomavirus.
After infection, genital warts do not form immediately. When they merge, they increase in size, which can cause unpleasant consequences (for example, injuries and bleeding). On palpation, all formations are painless, mobile, the skin around them is not changed.
Also, condylomas appear on the pubis, inner thighs, in the inguinal region. A man may experience additional symptoms:
Complications:
The appearance of genital warts in the genital area does not affect the reproductive health of a man. However, he becomes contagious to his sexual partner. That is why, if unclear formations are found on the genitals, you should immediately contact a dermatovenereologist or urologist.
4.2. warts
In men, warts can form:
The cause of such formations is most often papillomavirus types 1, 2, 4, 27 and 57. They have different affinity to tissues: with vulgar warts, HPV types 1, 2, 4, 26, 27, 29, 41, 57, 65, 75-78 are more often detected, with plantar warts - 1, 2, 4, 60, 63, with flat - 3, 10, 28, 38, 41, 49.
5. Rare forms of human papillomavirus infection
Rare pathologies include Bowen's disease, bowenoid papulosis, penile cancer.
5.1. Bowen's disease
It is characterized by the formation of spots with a velvety surface and uneven outlines, located on the skin or mucous membranes. Their color on the mucosa is bright red, on the skin it is gray-brown. The size and number of formations can be different. In men, similar spots form on the penis, hands, head and are caused by 16, 18, 31 and 34 HPV types.
The formation is usually located inside the epidermis, but can subsequently transform into invasive squamous cell carcinoma.
5.2. Bowenoid papulosis
Manifested by multiple papules (1-30 mm in diameter) with a smooth surface and jagged edges on the head or body of the penis. It occurs in persons of any age category, more often in old age against the background of infection with 16, 18, 34, 39, 40, 42, 45 types of papillomaviruses.
Bowenoid papulosis has a benign course, prone to regression. However, in some cases, the disease can transform into cancer.
5.3. Penile carcinoma
Highly oncogenic HPV types (namely 16 and 18) under certain conditions lead to malignant degeneration of the epithelium, dysplasia and cancer.
Bowenoid papulosis, Bowen's disease, Keyr's erythroplasia, balanitis obliterans contribute to the appearance of a malignant formation of the male genital organs. Most often, the primary defect is formed on the head, less often on the sheets of the foreskin and goes unnoticed. It is a flat or exophytic formation, which gradually grows in depth.
Features of the malignant process are:
6. Diagnostic methods
Diagnosis of papillomavirus infection is reduced to the initial examination of the affected area, the sampling of biomaterial for research (smear from the urethra, biopsy of the formation). The received material is being investigated. Tests can determine not only the presence of HPV, but also the genotype of the virus, as well as the viral load.
Less commonly, an enzyme immunoassay is performed to detect antibodies to the human papillomavirus in the patient's blood (class G and M immunoglobulins).
7. Treatment and prevention
In the treatment of HPV infection, the following points should be noted:
To remove genital warts, papillomas and viral warts, the following methods are more often used: excision with a laser, electric knife, scalpel, removal with liquid nitrogen.
Chemical methods are also used: exposure to nitric, trichloroacetic acids and their combinations. In recent years, drugs such as Mardil Zinc Max, Duofilm and Solcoderm have appeared on the pharmaceutical market. With their local application, local necrosis of the papilloma and its spontaneous destruction develops.
With multiple large condylomas, precancerous conditions, combined therapy and dynamic monitoring are performed.
The effectiveness of treatment largely depends on the chosen scheme, the age and state of immunity of the patient, and the size of the lesion.
Prevention of HPV infection in men is reduced to a decrease in the number of sexual partners, the use of barrier contraceptives (condoms), regular medical examinations by a urologist,.
Human papillomavirus is a large group of related viruses, each of which is assigned a personal digital code. Each species has a unique DNA set, and this characteristic distinguishes it from others and determines its properties.
The disease is transmitted with the same frequency to both men and women, but according to statistics, every third case of the disease in women occurs without the manifestation of acute clinical signs, while in men the symptoms are almost always pronounced.
To date, experts have identified about 600 human papillomaviruses, divided into 40 systematic species. However, only some of them are dangerous for human health.
The international classification of diseases ICD-10 assigns the human papillomavirus code B00.7.
More than 40 strains cause outgrowths in the genital and perianal region, but the biggest danger lies not in the cosmetic effect, but in the likelihood of tumors degenerating into malignant tumors. Each species has its own degree of oncogenicity. According to this degree, they are divided into the following groups:
- non-oncogenic(almost never cause cancer);
- low oncogenic(cause malignant processes in rare cases);
- oncogenic(relatively often provoke the onset of a cancerous process).
It is well established that even highly oncogenic groups are more likely to give rise to malignant tumors in the presence of a genetic predisposition, and for men who do not have such a predisposition, the risk is minimized.
Ways of infection
To be activated in the body, the pathogen must penetrate the cells and become activated. But not always contact with a pathogen means the onset of the disease. It depends on the degree of resistance of the immune system to viral agents: sometimes even with daily contact, protection can be so effective that the disease will not develop.
There are four main routes of transmission of an infectious agent:
- Sexual contact. This way is implemented most often and is classical. The causative agent is equally likely to be introduced into the epithelial tissue during all types of sex: vaginal, oral or anal. In addition, the transmission of the virus occurs with the same success without sexual intercourse, but during kissing.
- Contact-household way. The rarest method of transmission. Since the virus is able to live for a short time after leaving the body in the external environment, if there are minor injuries on the skin, it can infiltrate while using the personal belongings of a sick person (dishes, bed linen or underwear, personal items). Public toilets, transport, saunas are areas of increased risk of infection with human papillomavirus, since the pathogen is contained in all physiological fluids.
- Transmission from mother to child. Infection occurs during the perinatal period or when the fetus passes through the birth canal. Transmission of the virus does not necessarily occur, even in the case of a high titer of the presence of microorganisms in the mother, sometimes infection is not observed.
- Autoinfection. Secondary spread of the infection throughout the patient's body when shaving or after transferring the microbe by hand from the lesions to new foci.

Experts believe that papillomavirus is present in the bodies of 50% of people, but in the majority it takes the form of carriage and does not provoke the onset of symptoms.
Factors that increase the likelihood of infection with the papillomavirus:
- early entry into sexual activity;
- frequent change of sexual partners and neglect of methods of barrier contraception;
- age 17-25 years (peak sexual activity);
- sexual contact with a partner who has previously had any sexually transmitted diseases (due to the high association of HPV with other sexually transmitted diseases);
- any disease with a chronic course;
- taking glucocorticosteroids or cytostatics (anticancer drugs);
- obesity;
- thyroid dysfunction;
- impaired insulin metabolism;
- lack of vitamins, especially group B.

Any deterioration in immunity and immunoreducing factors dramatically increase the chances of the pathogen to invade and activate in the body.
How the disease develops
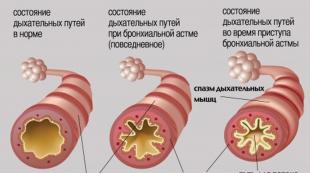
Once ingested, the microorganism enters the bloodstream and spreads throughout the body. Immediately after entering the target cells, it begins to actively integrate its DNA strand into the cell helix. The DNA of the virus includes a new genetic program in the cell, designed for rapid division. Due to unlimited divisions, outgrowths characteristic of the human papillomavirus appear on the skin.
The course of the disease is divided into several stages:
- Latent (hidden) period. There are no symptoms during the incubation period, so the patient himself does not know about the onset of infection. Despite the absence of clinical manifestations, a man is able to infect his partner during sex. The incubation period lasts from a couple of months to several years, until the immune system won't get stressed.
- Beginning of the active stage. By this time, the pathogen increases its presence in the cells of the body so much that it provokes the appearance of the first symptoms.
- Stage of active progress. All manifestations during this period occur very pronouncedly and increase intensively.
After reaching the clinical maximum, the disease develops in one of the possible directions:
- complete self-healing of the body with the final disappearance of all signs of infection;
- slow flow or stop the development of outgrowths (the infection does not go away, but does not progress);
- the rapid progress of all symptoms, the occurrence of secondary infection, an increase in the area of lesions;
- transition to a malignant course.
Outgrowth types
The appearance of formations, their size, shape and number in HPV are associated with the strain of the pathogen, since all manifestations of the infection depend on its genetic set.
All such formations are included in the endophytic or exophytic groups.
Endophytic formations
Such formations grow deep into the epithelium or skin, so sometimes they are poorly visible during examinations. They can be located both under the very surface of the covers, and penetrate to a sufficient depth. They have a stem or spine that tends to elongate over time.
Endophytes are represented by intraepithelial warts that affect the deeper layers of the dermal tissue. These warts are most often found in the groin. They have a convex top, smooth edges and a color that does not differ from the rest of the skin. After the appearance, they do not cause pain, itching or other uncomfortable sensations. In addition to the inguinal zone, they can be localized on the feet or skin of the palms.

Exophytic formations
They clearly protrude above the general level of the integumentary layer and are characterized by external growth.
External outgrowths are divided into:
- papules. These outgrowths slightly rise above the epithelium and form flat structures with an uneven top. In color, they sometimes do not differ from the skin, and sometimes they are somewhat darker than the surrounding tissues. Most of them are localized on the soles of the feet, on the face and torso.
- Flat warts. Characterized by rapid growth. Their appearance is accompanied by severe itching and burning. When palpated, they are found as fairly solid outgrowths. In the last stages, flat warts cause significant damage to the surrounding tissues.
- Pointed warts. They resemble columns rising above the level of the mucosa. The most common site of occurrence is the glans penis and coronal sulcus. Less commonly, the shaft of the penis, the perianal zone, or the rectum are affected. Condylomas can be located singly, and can form large groups. Sometimes their presence is accompanied by a sharp putrid odor.
In addition to endophytic and exophytic forms, there is also a mixed species - Bushke-Levenshtein formations. It is characterized by rapid growth in two directions - above the level of the skin and with penetration into the deep layers. Always have a significant size and cause periodic relapses.

All types of growths can be single or group. At the same time, there is a direct trend towards a deterioration in the condition of a man and an increase in discomfort with an increase in the area of the lesion. Significant groups may break, bleed, attach secondary infections and get wet.
Manifestations and symptoms
The appearance of the first symptoms means the end of the incubation period of the infection.
Warts or condylomas form in several stages:
- in the lesion, there is a slight inflammation and itching;
- within a few days, the skin or epithelium becomes covered with a small rash with or without liquid content;
- bumps or warts gradually increase in length or width;
- the appearance in the immediate vicinity of new rashes, which also turn into neoplasms.
The locations of the lesions depend on the way the pathogen enters the body and on the genetic set of the strain. Localization can vary greatly:
- most often - the penis;
- crotch;
- scrotum;
- anus;
- internal cavity of the urethra;
- epithelium of the oral cavity;
- face;
- armpits
- torso (back and sides);
- feet and palms;
- mucous eyes.

In the event that the neoplasm grows significantly inside the urethra, dysuria, bifurcation of the jet during urination and frequent urge to go to the toilet can be observed.
With the formation of such structures in the rectum, bleeding after defecation can be observed.
In addition to neoplasms, the following symptoms may be present:
- severe itching in the lesion;
- feeling of heaviness in the perineum;
- wetting of outgrowths;
- unpleasant putrefactive odor of affected areas.
A man may feel overwhelmed, fatigued, headache, fever and other signs of severe intoxication.
With the localization of papillomas on the penis, sex becomes painful, which makes it necessary to avoid sexual intercourse.
Often there is simultaneous infection with different strains of HPV, which aggravates the clinical picture and makes the symptoms as complete as possible.
Diagnostics
After discovering suspicious signs in himself, a man needs to contact an andrologist, dermatovenereologist or urologist.

During the initial examination, the patient's complaints are clarified and how much time has passed since the symptoms were detected and what is the dynamics of the disease. Next, the doctor conducts an initial examination and determines the location, intensity, size, color and condition of the neoplasms.
Advanced diagnosis of human papillomavirus consists of the following tests:
- PCR analysis. For research, scrapings are made from the skin or mucous membranes of lesions, and mucus is also taken from the urethra. In this case, the man should not visit the toilet for as long as possible so that the microorganisms are not carried out with the urine stream. This method allows not only to determine the presence of the HPV pathogen, but also to recognize its strain, which will allow you to know the level of oncogenicity.
- Digen test- an ultra-sensitive modern method that allows you to track not only the presence of an infectious agent, but also evaluate its possible consequences. The technique makes it possible to predict the development of the disease and complications with a high degree of probability.
- Anoscopy- the anus is subjected to a detailed examination through a magnifying technique to detect genital warts or warts in the anal area.
- Serological analysis for the determination of antibodies to HPV in blood serum.
- Histological and cytological method. For research, samples of outgrowths are taken and examined under a microscope after staining with microbiological dyes.
- smears from the urethra and from the anus for oncocytology and detection of atypical cells in the samples.
Timely diagnosis can significantly reduce the treatment course, achieve quick results and complete recovery.
In the video, a dermatovenereologist tells in detail about the examination of men for STDs, using a model of male genital organs as a good example.
Treatment
The problem requires not only the removal of cosmetic signs, but also a more comprehensive approach that will avoid a recurrent course of the disease.
Therapy has the following goals:
- stopping the virus;
- getting rid of neoplasms;
- increase in the immune status of a man.
Methods of combating human papillomavirus are divided into destructive and pharmacological.
Destructive Methods
These methods quickly alleviate the patient's condition with HPV in case of large lesions, growths in the urethra or anus, because after reaching a certain size, warts and condylomas lose their ability to heal.
You can eliminate neoplasms using the following methods:
- Excision by the surgical method. Requires local, and often full anesthesia. After removal of the formations, the cavity is sutured with a surgical suture. Previously, surgical excision was the main way to solve this problem, but due to frequent postoperative bleeding and complications, this method is now rarely used.
- Cryodestruction. The outgrowths are exposed to liquid nitrogen, which freezes out the cells of the nodules, during which the tissue proteins are destroyed. After that, the heads dry out and fall off. The positive point is the absence of the need for anesthesia and complete cleanliness of the skin without scarring after healing.
- Laser therapy. The technique resembles a cosmetic procedure. The effect of anesthesia is most often achieved by applying a special topical cream. The device points the laser to the affected area, and the beam has a destructive effect on the stem or root of the neoplasm. The disadvantages of the method are pain, high price and the frequent occurrence of scars or scars after the procedure.
- Electrocoagulation. This method is affordable, but painful. In order to reduce these manifestations, local anesthesia is given, but sensitivity is still present. Under the action of current in unwanted cells, heat, which causes cauterization. After a few days, scabs remain, which fall off with the formation of scars.
- Radiosurgery. The radio wave type electrode eliminates large and medium growths with pre-treatment of the skin with antiseptic agents. This technology is the most modern and non-contact, which virtually eliminates complications. Traceless healing of wounds is observed in record time - in a day. The only disadvantage of the technique is the high cost.
- Chemical coagulation. The technique has limitations in application and is suitable only for medium-sized mergers. Cell death occurs after contact with a potent chemical reagent based on highly concentrated alkalis or acids. Since a chemical burn is provoked at the site of exposure, scars and scars appear after the procedure.

Treatment should not be limited to destructive methods, since after their independent use in almost 30% of cases, a relapse occurs after a certain time. Therefore, radical methods must necessarily be supplemented with medications.
Pharmacological methods
These methods involve getting rid of small benign growths caused by HPV. Therapy with the use of pharmaceutical preparations can be carried out on an outpatient basis under the guidance of the attending physician. It is aimed at eliminating small benign growths caused by HPV, stopping the virus and improving the immunity of a man. For this, the following groups of drugs are prescribed:
- Pharmacy medicines for the treatment of growths of necrotic action. For a certain number of days, it is necessary to point the agent to a wart or warts, avoiding contact or spreading of the drug on healthy tissues. After the prescribed course, a break in cauterization is made, after which the course is repeated again if the growth has not fallen off. The means used for these purposes are Epigen, Panavir, Kondilin, etc.
- Antiviral drugs. They are used topically or orally for systemic effects on the entire body. The length of the course is determined by the attending physician. For antiviral effects, Realdiron, Acyclovir, Fenistil, etc. are prescribed.
- Adaptogens and immunomodulators. These drugs perform the function of preventing relapses and are prescribed after the use of antiviral agents. Cycloferon, Podophyllin, Viferon, Likopid, Immunomax have a significant effect.

Sometimes, in parallel with taking immunomodulators, multivitamin complexes are prescribed.
Permanent immune protection after the transferred human papillomavirus is not developed, therefore, after the next contact with a sick person, infection occurs again.
At the end of treatment for high oncogenicity papillomavirus, repeated tests must be taken at intervals of 3 months, and in the case of low oncogenicity, once a year.
Consequences and complications after HPV
Left untreated for a long time, HPV can cause serious consequences for a man's health. The same happens in the case of a weak immune system, unable to resist the destructive processes caused by the presence of the virus in the body.
The most common complications:
- Development of secondary infections on lesions that were mechanically damaged. This provokes the occurrence of deep long-term healing ulcers in the perianal region, festering wounds and balanoposthitis.
- Infectious infection of the urinary tract and viral-bacterial urethritis. These complications can cause serious violations of urine excretion and its stagnation in the body, followed by intoxication.
- Appearance of hemorrhoids in the rectum and paraproctitis with the localization of large growths in the anus.
- Weakening of the immune system. The disease affects the immune system, making the body unstable in the face of any pathologies and stresses. Colds take a protracted character, are difficult to cure and more often give complications.
- Sexual dysfunction due to physiological and psychological factors. Physiological include violations of the normal functioning of the seminiferous tubules, damage to the scrotum and inguinal region, and increased pain during sex. Psychological disorders include forced renunciation of sexual life, which entails a violation of the emotional background.
- The development of a special form of a malignant tumor, called squamous cell carcinoma member. Most often, it affects the upper part of the head of the penis, which, in the course of progression, destroys the cavernous bodies and the head, causes severe bleeding and can result in complete necrosis of the penis. Due to the active supply of blood to the penis, cancer metastasizes early to other parts of the body. For therapy, a surgical method of getting rid of the tumor and courses of chemotherapy are used.

Prevention
Paying attention to the consequences that pathology can cause, prevention becomes especially important.
There are 2 types of HPV prevention: specific and classical (general).
specific
The method is quite new, but has already proven its effectiveness. It involves vaccination. special preparations quadrivaccines with commercial names Cervarix or Gardasil. This vaccine is not active against all strains, but is effective against the four main ones that cause growths to degenerate into malignant structures.
Vaccination is undertaken until the moment of illness only in healthy people, if a man has already become infected with HPV, then vaccination is useless.

Vaccination is carried out in 3 stages, 2 and 6 months after the first injection.
General
To prevent the disease, the following measures must be observed:
- mandatory use of barrier contraceptives (it must be remembered that these funds do not guarantee complete safety, but significantly reduce the risk of developing the disease);
- compliance with the requirements of personal hygiene and sanitation;
- having a permanent sexual partner;
- systematic examination by an andrologist once a year;
- increase the immune forces of the body;
- rapid cure of pathologies of the pelvic organs.
In addition, it is necessary to exclude irrational nutrition, stressful situations, and ensure a normal rest regimen.
Compliance with all the rules of prevention will help maintain health and prevent the development of serious consequences.
HPV in men is one of the most common diseases modern world. According to studies, 8 out of 10 people on the planet are carriers of the virus. To get answers to the questions of how dangerous HPV is for men and what consequences the disease can lead to, it is necessary to understand the features of the development of papillomavirus.
The main sign of the presence of the human papillomavirus is the appearance of warts, papillomas and condylomas on the skin and mucous membranes of the body. Warts and papillomas do not pose a clear threat to human health, while warts located in the genital area and anus can cause significant harm.
On the initial stage Infection, a man may not be aware of the presence of HPV in the body. The infection is dormant and does not manifest itself in any way while the immune system is working normally. As soon as it weakens, the virus is activated, growths appear on the body.
With the penetration of HPV into the mucous membrane of the external openings of the urethra or rectum, genital warts are formed.
Causes of infection with the virus and ways of transmission
Human papillomavirus infection appears in men only after infection from another person. Infection occurs in three ways - during sexual intercourse, from mother to child at birth, by contact-household.
Protected sex is not a barrier to HPV infection. The cells of the virus are so small that they can easily penetrate any barriers, including latex.
Entrance gates for infection are microscopic lesions on the skin or mucous membrane, which a man may not see. Such microcracks are normal during sexual intercourse. To a greater extent, they occur in the anus. To a lesser extent, the mucous membrane of the vagina is affected. The cervix, in the presence of erosion, is 100% affected by HPV. The head of the penis is the least susceptible to injury.
You can get HPV without intimacy. The infection easily enters the body in public places. Common routes of household transmission:
- use of strangers hygiene supplies(towels, washcloths, razors, scissors, tweezers);
- wearing someone else's clothes and shoes;
- sharing dishes;
- walking barefoot on the beach;
- visiting the pools;
- baths, saunas, sports locker rooms;
- lack of sterilization of salon tools;
- handshakes with carriers at the stage of exacerbation of the disease;
- touching the growths of the wearer.
The human papillomavirus is one of the infectious infectious diseases. Not a single person on the planet is immune from infection. Strengthening immunity eliminates the likelihood of HPV activation. The appearance of growths is observed after prolonged illness, taking antibiotics, hypothermia and stress. This can happen as a result of beriberi, debilitating mental and physical activity, hormonal disorders. Drinking alcohol and smoking only increase the likelihood of immunodeficiency.
Is the virus in the body dangerous for a man and possible consequences
The danger of HPV depends on the strain that has entered the body of a man. Modern medicine distinguishes 4 types of genotypes - non-oncogenic, with a low degree, with an average degree, and highly oncogenic types. The former are practically harmless to the human body. These include common warts, hanging papillomas, plantar growths. They can be dangerous only in cases of abundant growth, when the integrity of tissues is violated skin. This is observed most often in people with severe immunodeficiency. Most often, single warts appear and cause only aesthetic discomfort.
Oncogenic strains are characterized by the manifestation of growths in the genital area and anus. Such a phenomenon can be considered dangerous. Warts damage leads to bacterial infection. A person is in pain when going to the toilet. The secretions may contain blood impurities.
Without timely comprehensive treatment, you can face a number of unpleasant and dangerous consequences:
- inflammatory process of the genitals;
- bacterial diseases of the genitourinary system;
- proliferation of formations - papillomatosis;
- painful urination, stool;
- damage to the integrity of the skin and mucous membrane of the intimate area.
Men are more fortunate than women and are much less likely to have cancer. According to statistics, there are 1 man for every 3 sick women. But it is not recommended to exclude the possibility of developing a dangerous disease and refuse full-fledged treatment.

Why often a man is only a carrier of the virus
Women's and men's bodies are equally affected by HPV. Men are more likely to be carriers of the disease than to face external symptoms. This is difficult to explain, the stronger sex is prone to the occurrence of viral formations in the groin area.
Women are subject to changes in the functioning of the body. A decrease in natural protection in women is observed before each menstruation, at the stage of hormonal imbalance, during pregnancy. For this reason, women often experience symptoms of candidiasis. Not important for the development of cancer. The main factor is damage to the epithelium of the cervix in the area of erosion (non-healing wound) HPV is introduced and feels quite at ease. Erosion is converted into dysplasia, HPV accompanies the process of malignancy of the cervix.
The protective function of the body of a man is stable. Only acute diseases, long-term drug treatment or serious exposure to external factors can provoke suppression of the immune system.
A man is less likely to become infected with papillomavirus, since the structure of the penis ensures the integrity of the skin. The penis suffers less friction during contact than the female vagina. The exception is passive homosexuals, whose risk of infection is higher than that of women.
Methods for diagnosing the human papillomavirus in men
Diagnostic testing is an important step in the treatment of HPV. Thanks to timely diagnosis, it is possible to determine not only the presence of HPV, but also to recognize its type, concentration or load on the immune system.
Diagnostic measures begin with an examination in the urology room. In the presence of growths in the anogenital zone, the doctor can easily recognize HPV.
To confirm the diagnosis, the patient is prescribed a test for laboratory testing. A smear for PCR and blood for ELISA is subject to study.
The main test for detecting HPV is cell sampling. The material for men is a scraping of the epithelium from the urethra. The doctor inserts a special probe into the urethral canal, after extracting the biomaterial, applies it to a glass slide and sends it to the laboratory. To obtain reliable information, screening and the polymerase chain reaction method are carried out. Under laboratory conditions, perform the Digene test.
Enzyme-linked immunosorbent assay (ELISA) is carried out by examining blood. To confirm the diagnosis, a specific antigen is detected - a protein that is produced by the immune system in response to the activity of the infection.
Histological examination is performed with suspicion of oncology. The biopsy specimen is a fragment of the removed condyloma. The structure of tissues is being studied. The method allows you to identify changes in a man in the early stages.

Methods of treating HPV in a man
HPV treatment consists of a set of measures that are aimed at suppressing the activity of the infection and restoring the functioning of the immune system. Therapy includes taking antiviral, immunostimulating, vitamin preparations and removing growths.
For young men, in isolated cases of wart formation, only removal can be carried out, the immune system of a young organism can self-heal. For older people, a single-component treatment regimen is not enough.
A popular method of getting rid of warts is hardware treatment:
- laser excision - the growth is burned out with a laser beam;
- cryodestruction - the destruction of papilloma tissues with liquid nitrogen;
- diathermoelectrocoagulation - burning out due to electric current;
- radio wave method of removal - excision with a radio knife.
Removal in men can be carried out by exposure to pharmaceutical drugs. The drugs are intended for home use. Most of them cauterize papillomas, some have not only keratolytic, but also antiviral effects.
Effective antiviral agents for combating HPV are:
- Isoprinosine;
- Immunomax;
- Viferon;
- Cycloferon;
- Allokin Alpha;
- Groprinosin;
- Aldara;
- Panavir.
The drug is prescribed by the attending physician individually. The doctor needs to assess the patient's condition and the characteristics of his body. Self-selection of drugs is undesirable.
Prevention of infection with the virus for men
Preventing viral transmission is difficult given the contagious nature of the disease. You can reduce the risk of infection. It is necessary to pay attention to several important things - personal hygiene, protecting the skin in public places, the culture of sexual life and maintaining immune defenses.
It is unacceptable to use hygiene devices of a stranger. Shoes should be worn in places where other people prefer to walk barefoot.
Verified partner - The best way HPV prevention. The more sexual relationships a person has, the higher the risk of the disease.
Modern medicine involves the use of papillomavirus vaccines not only for adolescent girls, but also for boys, in order to prevent the spread of morbidity in the population.
The human papillomavirus in men can lead to the development of dangerous complications. You should not delay contacting a doctor. HPV in women and men should be treated as soon as symptoms occur. The sooner the patient seeks help, the more effective the treatment will be.
HPV in men develops only when the virus enters the human body, but it brings a lot of inconvenience, as it leads to the spread of neoplasms throughout the body. They are not especially dangerous, but can be transformed into malignant tumors.
That is why any young or old man should be more attentive to the appearance of human papillomavirus infection in his body. It is necessary to understand why warts appear on the skin and understand how to get rid of them correctly.
The human papillomavirus in men signals that it is present in the human body if a rash appears on their body in the form of flat-type warts on the skin. Scientists have long found that neoplasms can appear much less frequently than in the female.
Manifestations of papillomavirus are dangerous because it can constantly mutate, causing malignant tumors in people. In a latent state, it tends to be stored in the body for many years, without showing itself in any way.
Most often, papillomavirus manifests itself in men who are already eighteen or twenty-five years old, because they lead an active sex life and receive microtrauma. It is through small cuts and wounds that an insidious disease enters the body, actively multiplying on the mucous membranes.
Patients often state the fact that flat formations are covered with:
- face;
- mucous membranes of the mouth and nose;
- mucous on the genitals;
- armpits
- soles of the feet;
- back.
HPV in a particular man in the photo can bring a lot of problems and discomfort, since genital warts are most often located on the penis, preventing them from leading a normal life. Warts in the penis area are often damaged by underwear, bleed and give off a rotten smell.

It will be more terrible if he penetrates into genitourinary system, blocking the opening of the urethra, as urine ceases to be excreted from the body.
Papillomavirus infection in men enters the body, due to its small size, through any wounds and cracks. Transmitted in several common ways:
- through unprotected sexual contact;
- household way;
- during the birth process.
In sixty percent of cases, the HPV virus in men was the result of contact with an infected sexual partner. It has not yet been established in which species the highest danger lies, since it is realistic to catch the infection not only in the traditional way, but also in the anal and oral way.
HPV is also dangerous because a condom cannot protect it from transmission, since microscopic particles easily enter the vagina or anus through the pores in the latex. It is not easy to protect yourself from infection, because the virus most often enters the body through kisses and saliva on a cigarette smoked for two.
The household route of infection with papillomavirus infection also occurs frequently, since the virus is dangerous in water and in the atmosphere. HPV symptoms in men may occur if:
- visits to the sauna or swimming pool;
- haircuts at the barbershop;
- manicure or pedicure in the salon, where they do not monitor the cleanliness of tools;
- surgical intervention in surgery, manipulation room, dentistry and antenatal clinic.
Many articles by leading medical luminaries are devoted to what can be transmitted from an infected mother to a newborn baby. This means that even a newborn boy is, against his will, a potential carrier of HPV.

The causes of infection with a viral infection can be:
- weakening of the immune system;
- manifestation of any types of diseases that are sexually transmitted;
- active life, which implies stress and emotional stress;
- constant risk of physical and mental overload.
The diagnosed human papillomavirus in men, the symptoms of which were listed above, most often affects the body if it is weakened by unbearable loads. The rapid development of viruses allows you to quickly populate the mucous membrane of the genital organs, intestines and mouth, and then rapidly change the structure of tissue cells.
The main symptoms of the human papillomavirus
If he finds new and new flat warts on his body, then we can say that he was struck by a viral infection.
It is not difficult to find articles by experts about what HPV is in a man, what symptoms and treatment are typical for him, but it is stated that there are plenty of strains of the virus.
Only a professional doctor can correctly diagnose and cure the disease. The main signs of a viral infection that are diagnosed after examination include:
- the appearance of convex neoplasms;
- painlessness of warts;
- sharpness of condylomas, which appear in the inguinal region and on the head of the penis;
- the presence of spikes on the soles of the feet, the main features of which
unbearable itching and pain when moving, roughness and necrosis of plantar tissues; - the occurrence of papulosis, that is, painful formations on the penis, which are characterized by a pinkish tint.
The human papillomavirus in a man in the photo often manifests itself in the form of large red spots that affect the head of the phallus and cause discomfort.
Human papillomavirus has features if it affects the inguinal region in men, because it negatively affects potency and erection. A person is often unable to understand that he is infected, because at the initial stage the disease proceeds without any symptoms and does not bring pain.
The consequences can be deplorable, since one of the cells can degenerate into a malignant tumor and cause oncology. When the first signs appear, you should immediately contact a specialist to find effective drugs.
Features of HPV diagnostics
How to treat papilloma in men faster and more comfortably can be told by a dermatologist who has an appropriate diploma. Before prescribing effective medications, the doctor will listen to all the patient's complaints, examine him and clarify the need for advanced diagnostics. This is done to determine the form of papilloma in an individual man, the treatment of which will depend on its severity.
The main methods of this diagnosis are usually referred to:
- clinical and general blood test;
- examination of tissues for cytology;
- taking smears from the urethra;
- ureteroscopy;
- PCR diagnostics to identify and cure complex strains;
- cytology of tissues of the anus and rectum;
- a variety of screenings to determine the clinic.
In the event that the neoplasm requires surgical intervention, then a decision is made to remove it surgically, therefore, an experienced surgeon continues to lead the patient.
How to treat HPV in men, if the neoplasm turned out to be malignant, an oncologist, not a dermatologist, will think.
It is clear where the human papillomaviruses in men came from, how the treatment is also clear, but it is worth clarifying that there is never a complete cure for an insidious disease.

When all the reasons are clarified and a strain is detected, then experts will try to reduce the activity of HPV reproduction and eliminate the problems that the papillomavirus has already brought in men.
If the good quality of the papilloma is proven, then treatment is carried out only when it is really necessary. In other cases, everything remains as it is, since the removal of the wart can lead to its degeneration into a malignant tumor.
The scheme of the conservative form of treatment of the disease is simple and consists in the use of only drugs aimed at:
- increased immunity;
- fight against viruses;
- blocking cell division;
- launching the synthesis of interferons;
- reduced growth of viral cells.
All doses of the drug are calculated by the dermatologist individually for each patient.
If treatment does not help, then after some additional analysis of how HPV manifests itself in most men, the removal of one or more neoplasms will be prescribed.
The surgeon will decide on his own whether to use a traditional scalpel or resort to sparing methods using:
- excision with a radio knife;
- laser removal;
- electrocoagulation;
- cryodestruction.
The method of classical papilloma excision with a scalpel is used for malignant tumors, after which small scars remain. The remaining four schemes are more modern, they relieve scars and bleeding. The place after removal of papillomas with lasers or a radio knife will be invisible, and the method itself will not cause complications.
The last two methods are painful, they cause discomfort, the rehabilitation process can be delayed for a couple of weeks.
Experts forbid tearing off warts on their own or cauterizing papillomas in men before adequate treatment occurs. Any damage to a flat wart in half of the cases can lead to its degeneration into a malignant tumor with all the ensuing consequences.
Prevention of papillomavirus in a strong half of humanity
Now it is clear how dangerous untreated HPV is for most men, so it is necessary not to start the course of the disease, but to consult a doctor in time at the slightest suspicion that the papillomavirus has entered the body.
To save money and time, it is worth doing HPV prevention.
Human papillomavirus and its negative impact on the reproductive system today is one of the most frequently discussed problems. What is the danger of infection with certain types of virus for women is well known. And what are the consequences of human papillomavirus infection in men?
Papillomavirus infection is one of the most common in humans. More than 95% of adult women and men are infected with some type of HPV or several at the same time. Moreover, the majority of people do not even know about the carriage of the virus and are clinically absolutely healthy. This infection is transmitted only by direct contact from person to person. The virus multiplies and lives in the epithelium of the skin and mucous membranes of the genitals, throat and mouth.
Properties and types of HPV
Today more is known 150 varieties of HPV. Virus different types causes various options infections of the epithelium: from simple warts to the appearance of cancer. Therefore, 3 types of papillomaviruses are distinguished, taking into account oncogenic risk.
- Non-oncogenic species- never cause malignant neoplasms. A virus of this type is either eliminated from the body on its own, or provokes the appearance of warts.
- HPV of low oncogenic risk- can provoke an oncological process in certain conditions favorable for it (extremely rare). These types of viruses are sexually transmitted and usually cause genital warts.
- HPV high oncogenic risk- very often provokes cancers mainly of the genitourinary system.
Methods of infection
HPV infection occurs only during direct contact with a sick person through the mucous membranes and skin with microdamages. The household method of transmission is quite common, since the papilloma virus can persist for a certain time in particles of desquamated epithelium.
 Infection with HPV types that affect the mucous membranes passes during sexual intercourse. Therefore, these types of human papillomavirus infection belong to diseases that are sexually transmitted, and are often combined with other similar infections (trichomoniasis, mycoplasmosis, chlamydia). The likelihood of high-risk HPV infection increases with the number of sexual partners and sexual activity.
Infection with HPV types that affect the mucous membranes passes during sexual intercourse. Therefore, these types of human papillomavirus infection belong to diseases that are sexually transmitted, and are often combined with other similar infections (trichomoniasis, mycoplasmosis, chlamydia). The likelihood of high-risk HPV infection increases with the number of sexual partners and sexual activity.
HPV infection of newborns is likely during childbirth with the development of anogenital warts or laryngeal papillomatosis in infants.
Symptoms of the human papillomavirus in men
Most often, HPV infection and symptoms in men, even with oncogenic types of infection, do not carry such serious complications as for women. In general, HPV infection is completely asymptomatic and does not cause any pain.
With strong immunity, the papillomavirus in men often remains in a latent form or is eliminated independently from the body.
Infection with non-oncogenic types of the virus in certain cases leads to the development of flat warts on the skin of the hands or papillomas in areas of the skin that are subject to friction with clothing (inguinal and axillary areas). These symptoms cause papillomavirus types 2, 3, 5. The appearance of palmar or plantar warts is likely, often very painful during pressure on the thickening of the stratum corneum of the skin of an irregular shape. They are caused by HPV type 1. These symptoms are equally common in women and men.
Infection with low-oncogenic types of HPV 6 and 11 occurs during intercourse with an infected partner and provokes the appearance of genital warts in the genital area and anus. This pathology is one of the most common symptoms of human papillomavirus in men. The disease may appear after a long (more than 4 months) incubation time. Most often, the source of infection cannot be established, since the virus in most people does not cause painful manifestations and is in a latent state.
 Genital warts are skin growths on a narrow stalk that resemble a comb or cauliflower in shape, most often painless. They are found in men in the region of the anus, coronal sulcus or foreskin. The location of warts is probably in the urethral canal, as a rule, combined with anogenital. May cause symptoms chronic urethritis and impaired urination.
Genital warts are skin growths on a narrow stalk that resemble a comb or cauliflower in shape, most often painless. They are found in men in the region of the anus, coronal sulcus or foreskin. The location of warts is probably in the urethral canal, as a rule, combined with anogenital. May cause symptoms chronic urethritis and impaired urination.
The laryngeal appearance (laryngeal papillomatosis), which is caused by HPV type 11, is usually observed in children under 7 years of age. Most often associated with infection during childbirth. But it can develop in adults infected through oral-genital contact. The first symptoms of laryngeal papillomatosis are swallowing disorders, soreness and hoarseness.
High-risk HPV in men can lead to throat, anal, or penile cancer.
In men, anogenital cancer is observed much less frequently than in women, carcinoma of the cervix. This is due to the anatomical structure of the reproductive system. The likelihood of contracting anogenital cancer will depend on the body's sensitivity to HPV, the state of immunity, and some other factors. For example, anal cancer is observed 20 times more often in men who have sex with men, as well as in patients with HIV.
 Signs of anal cancer are bleeding during bowel movements, itching, pain. In some cases, there are no symptoms at all. Symptoms of penile cancer are discoloration of the skin in the form of a spot or focus, thickening, later enlargement of the lymph nodes in the groin, bleeding and erosion.
Signs of anal cancer are bleeding during bowel movements, itching, pain. In some cases, there are no symptoms at all. Symptoms of penile cancer are discoloration of the skin in the form of a spot or focus, thickening, later enlargement of the lymph nodes in the groin, bleeding and erosion.
Cancers of the larynx and pharynx can sometimes be associated with certain types of HPV, but most of these cancers are associated with smoking and other causes. Typical HPV symptoms for laryngeal cancer in men are coughing, persistent sore throat, difficulty swallowing, hoarseness, or voice change.
Diagnosis of the HPV virus in men
When there is a suspicion of infection with papillomavirus, the doctor, in addition to visual examination, may prescribe the following diagnostic methods:

Often patients ask how and where to get tested for human papillomavirus? A man needs to come to the clinic to the appropriate doctor (urologist, dermatovenereologist, dermatologist), who will give a referral for an examination.
Treatment of papillomavirus in men
A man is obliged to conduct special treatment even in cases where HPV is detected only in his partner. In 80%, a man is affected by the virus through sexual contact, but in the early stages of infection of the body, clinical symptoms may not appear. Special drug treatment will help fight the virus and prevent it from infecting the skin.
Mandatory treatment of papillomas in men should be carried out with the manifestation of clinical symptoms:
- Pointed warts.
- papillomas.
- Polyps.
In this case, assign:
- antiviral therapy.
- Immunostimulatory treatment.
- Surgical removal.
 You need to know that the traditional drugs acyclovir and valaciclovir are drugs for the herpes virus. They have an antiviral effect, but do not give positive results if they are treated with the papillomavirus.
You need to know that the traditional drugs acyclovir and valaciclovir are drugs for the herpes virus. They have an antiviral effect, but do not give positive results if they are treated with the papillomavirus.
Means for immunostimulating treatment are licopid, derivative, thymalin. When prescribing any immunomodulator, the doctor needs to send the sick person for a special examination, with which it will be possible to choose the right remedy.
We must not forget that the immune system is a special mechanism, disrupting its work, you can suffer irreparable consequences. To strengthen the body, it is necessary to have the right therapeutic effect.
Special antiviral drugs must be prescribed before and after surgery. These remedies fight the cause of the appearance of neoplasms and make it possible to stop their recurrence. But keep in mind that the HPV virus cannot be completely cured, but only to stop its progression in the body.
In addition, we must not forget that when you use only one way to deal with papillomavirus, then you can not expect a positive effect. In this case, the treatment will be expensive and lengthy, and there will be practically no effectiveness.
How to treat HPV in men: different ways
Consider the main methods used to remove growths on the skin as a result of HPV infection:

It is believed that HPV is dangerous only for women, but in men, papilloma is also often noted. This virus can bring many problems, from just aesthetic to serious cancer. And even when a man himself is not sick, he can be a carrier of the infection and infect women. At the same time, the carrier of the virus, when his immunity turns out to be weak after a while, can get sick himself.